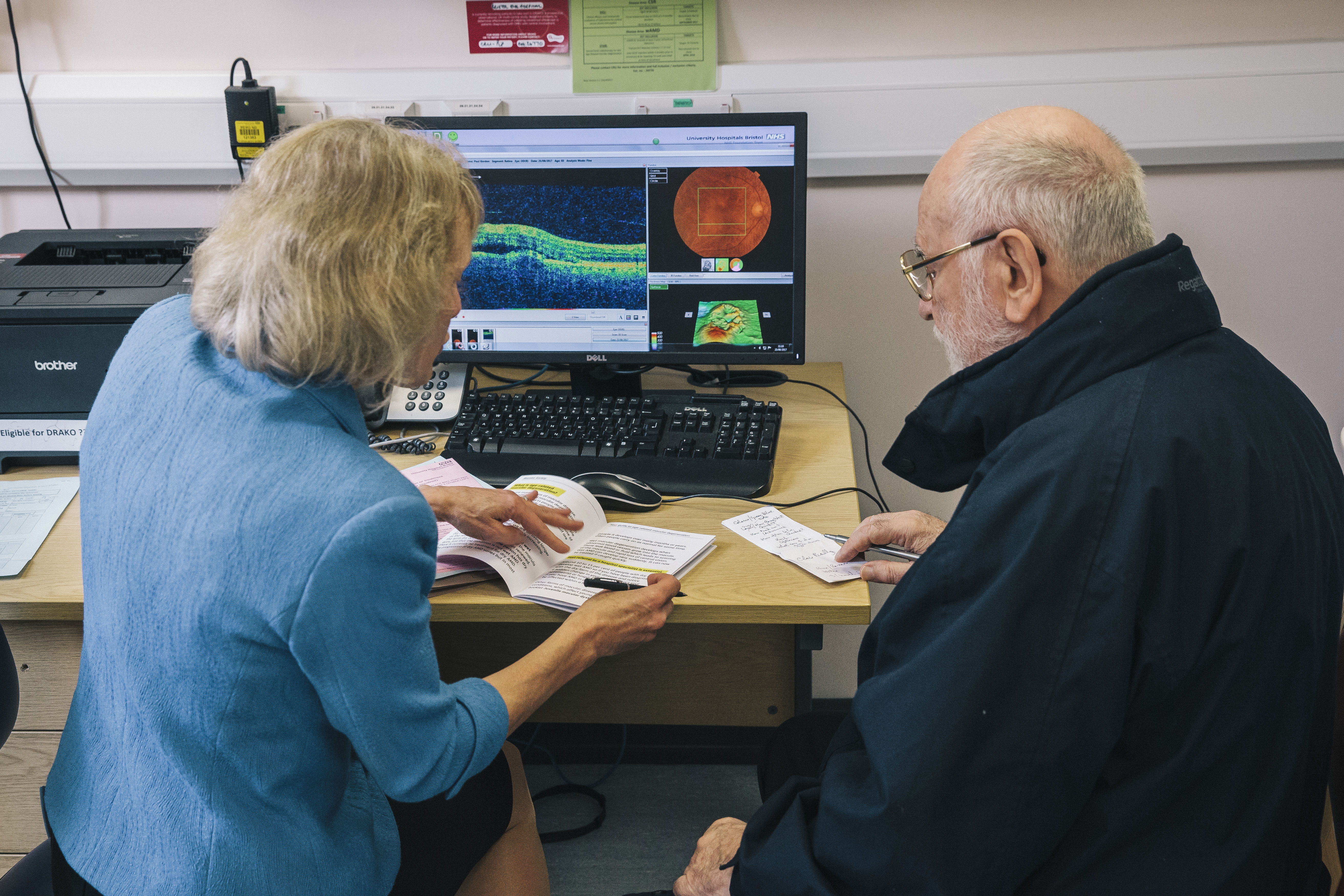
Communicate better with patients
The way you talk to patients about their macular disease can have a big effect on their mental health, and prognosis.
Whether you’re in private practice or the NHS, time with patients can be limited and the focus, naturally, is on providing the clinical care and treatment the patient needs.
However, the quality of communication with patients also affects outcomes. Patients’ experience of their disease, and their ability to manage it, can be improved by good communication.
Please remember that patients may be shocked by the news you have given and may not take in all the information. They may be too shy to ask questions or admit they have not understood what you have told them.
What do patients need?
- A clear diagnosis and explanation of the treatment available. If there is no medical treatment available, please do not say ‘nothing can be done’. This phrase is devastating for a patient to hear and not true; even where there is no medical treatment there are many other avenues to explore to manage life with macular disease. These include the use of low vision aids and technology.
- An opportunity to discuss their vision and how they feel about it.
- Accessible information they can take away to read later, possibly with family members or carers.
- Referral to low vision services as soon as vision starts to deteriorate, not at the end of any treatment programme or at the point where certification is possible.
- Advice on lifestyle and particularly smoking cessation if appropriate.
- Clear guidance on how to monitor their vision and what to do if they notice a change in it.
- Prompt advice on certification when appropriate.
You can support your patients by signposting or referring them to the Macular Society and our free practical and emotional support.
Not just a ‘nice to have’
There is evidence that taking these actions improves patient wellbeing and outcomes.
Preserving vision
A large survey of Macular Society members found that 44 per cent of respondents diagnosed after 2009 reported not receiving information on what to do if vision deteriorated. Lack of such information at diagnosis was significantly associated with registration as sight impaired.
Improving mental health
Good communication allows patients to express their fears and concerns. Many patients with macular disease suffer great emotional distress and need support and, frequently, therapy. This applies even in those patients who can be treated.
A study of wet AMD patients in Manchester found an unexpectedly high level of clinically significant, undiagnosed, depression in patients. Patients need holistic care, not just eye care.
Helping patients cope with the future
Most people with macular disease have dry aged-related macular degeneration (AMD). Research suggests that many patients feel they do not receive good quality information at diagnosis.
Diagnosis of dry AMD results in significant psychological burden for the patient and many fear ‘going blind’. Perceived impact on daily life may be considerable whilst measurable visual function remains reasonable and support is needed for patients, both directly following diagnosis and in the longer term.
Read more on these research results.
Preventing unnecessary anxiety
An often-overlooked side-effect of sight loss is visual hallucinations known as Charles Bonnet syndrome (CBS). This condition has been regarded as a transitory phenomenon of no clinical significance.
However, research with Macular Society members suggests that CBS is much more common than often thought and can last for many years. In a study of Macular Society members, one third of people with CBS experienced ‘negative outcomes’: intrusive or distressing hallucinations that interfered with daily life, or believing that the hallucinations were a symptom of a mental illness or brain disease such as dementia.
This fear was more common in patients who had not had prior warning of the possibility of CBS before experiencing symptoms.
Other professional resources 
Eyecare professionals are on the front line of the fight against macular disease. Whether you are a health, social care or education professional, we want to do everything we can to help you provide the best possible care and support for people with macular disease.
Preparing documents for visually impaired people 
We offer guidance to help professionals prepare documents for visually impaired people.
Get the latest news and advice from the Macular Society
To hear about life-changing research, treatments and tips for living with sight loss, subscribe to our monthly enewsletter today. Together we can Beat Macular Disease.
Sign up to our free email newsletter