Our research projects
Since 1987 the Macular Society has invested around £10 million in over 100 research projects. Each year we invite applications for research grants, PhD studentships and seedcorn grants which are assessed by our Research Committee.
Research grants
Research grants are for projects of up to three years duration and up to £300,000, which covers everything from laboratory chemicals to salaries.
PhD studentships
A PhD studentship funds a student to undertake a three year research project. The student submits a thesis for qualification of the degree, which is the highest level of academic degree attainable.
Seedcorn projects
A seedcorn grant is funding of up to £25,000 to generate preliminary data to advance innovative and novel ideas.
Fellowships
A fellowship is an award that provides funding for individuals to pursue research, study, training, or professional development.

Measuring visual pigment regeneration to track Stargardt progression
Researchers at Cardiff University are using a novel imaging technique, Imaging Retinal Densitometry (IRD), to track how the retina’s light-sensitive cells regenerate. This study aims to better understand Stargardt disease progression and support the development of new treatments by providing an objective measure of retinal function over time.
Find out more

Folding correction for Stargardt disease
Stargardt disease is often caused by mutations in a gene called ABCA4. Mutations cause the ABCA4 protein produced to fold incorrectly and be removed from the cell. This project looks at correcting the folding of the ABCA4 protein, to maintain the function and health of the macula.
Find out more

Finding early AMD changes using eye scans
Using long-term follow-up eye scans from a study into ageing, to understand what changes in scans may be early signs of AMD.
Find out more
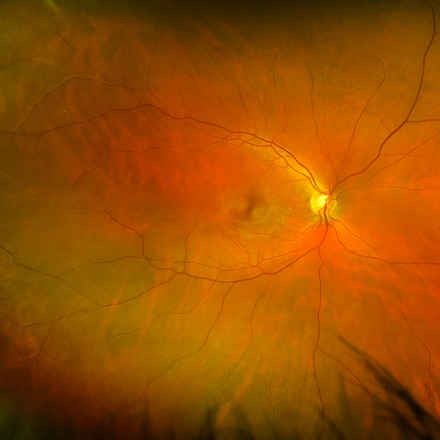
Maintaining the health of the blood vessels in the macula
Understanding how the blood vessels in the macula may play a role in AMD, and trying to find a treatment to maintain their health.
Find out more
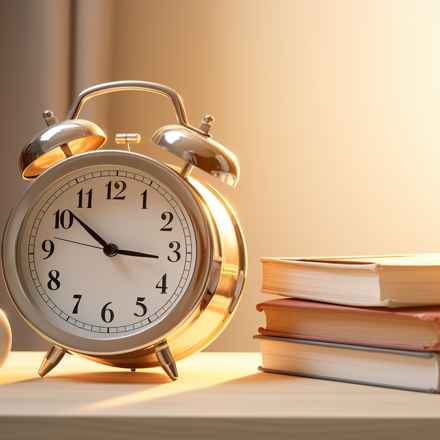
Shining new light on the body clock and retinopathy
Disruptions to our body clock can have an impact on our health, including links with eye damage for people living with diabetes. Dr Eleni Beli takes a closer look at these links, to understand more about how eye damage can develop and progress. Her research could uncover an innovative new approach to help people with diabetes avoid sight loss.
Find out more

A marvellous new approach to tackle retinopathy
High blood sugar levels can lead to damage to our eyes, known as retinopathy. Professor Karl Matter's research could provide valuable new insights to develop innovative approaches to protect blood vessels and prevent sight loss for people with diabetes.
Find out more