What to do after a macular disease diagnosis
Being diagnosed with macular disease can feel distressing, overwhelming, and leave you with many questions – not just about your eyes, but about what life will look like next.
You’re not alone. With the right knowledge and support, people diagnosed with macular conditions go on to lead fulfilling, independent lives.
This page will help you understand what to expect now and in the future, how to manage the emotional impact, and where you can find information and support to help you take the next steps with confidence.
What happens after a macular disease diagnosis?
When learning about a new condition it’s important to go at your own pace, but we can help you find out more about macular disease and what steps you can take.
Will my vision get worse right away?
Everyone experiences vision changes in different ways. Your vision may change quickly, or more slowly, depending on the type of your condition and how severe it is. Some forms of macular degeneration have treatments available that can slow down the disease and stabilise your vision.
Vision changes and sight loss can be distressing. But even with advanced macular degeneration, most people still have some sight. Macular disease affects the central vision, but the peripheral vision (what you see with the sides of your vision) isn’t affected. It’s also worth knowing that macular disease doesn’t cause physical pain.
What does treatment involve?
There are now treatments for some types of macular disease, but it depends on your specific condition. Treatment for macular conditions can be very effective, especially when treated early.
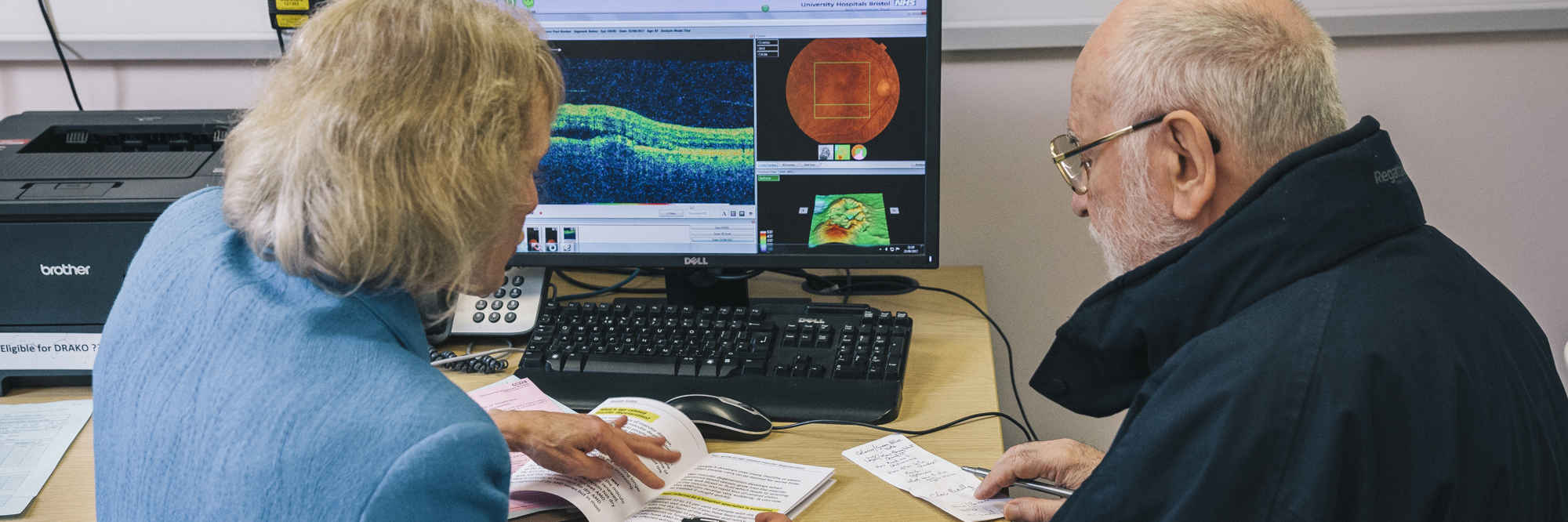
Who will I see for ongoing care?
You’ll typically continue to see your eye care professionals such as ophthalmologists, optometrists or specialist retinal consultants.
Alongside clinical care, the Macular Society offers helpline support, counselling, befriending and local support groups to guide you through the journey.
Can I still live independently or work?
Yes. Many people with central vision loss continue to live independently and work, especially with the right tools and adjustments.
We offer Skills for Seeing training, assistive technology tips and advice on working safely and legally, such as understanding DVLA driving requirements.
Newly Diagnosed To-Do List
Get to know what to do after being diagnosed with macular disease. Gain understanding, treatment information and emotional support with the Macular Society.
Telling other people
Learn how to share your macular condition with those around you, and understanding the practical and emotional changes it can bring. Telling other people about your sight loss will help to make those changes easier.
How you might be feeling
It’s completely normal to feel anxious, upset or isolated following a diagnosis. Many describe it like a grief process – experiencing emotions such as anger, denial or fear as part of adapting to sight loss.
Suzanne from our counselling team explains: “For many people there are and will be barriers to talking about how you're feeling. And these come up on a regular basis with our counselling clients.
“Some people don’t want to feel vulnerable and others may feel that speaking about their eyes or how they're coping may make it too real. They may just not be ready.
“Everybody has their own individual way of coping and what works for them.”
You may also feel frustrated or doubt your abilities, but reaching out – whether to our counsellors, peer support volunteers, or reading stories from others who have walked this path – can bring comfort, resilience and newfound strength.
More on looking after your emotional wellbeing
Discover how to care for your mental health when living with sight loss or supporting someone who is. Get self-care tips, emotional support, and services from the Macular Society.
Where to find help and support
We have a variety of resources and services to support you.
- Macular Society helpline: Free, confidential advice – call 0300 3030 111 (Mon to Fri, 9 am to 5 pm).
- Telephone counselling: Professional counsellors specialised in sight loss are available for one-to-one support.
- Befriending service: Friendly, regular phone calls from others who understand what you're going through.
- Support groups: Local and online groups offer friendship, advice and community. Find your local group or join condition-specific online groups.
- Treatment buddies: Telephone support for people who are anxious about their injections.
Practical steps you can take today
It’s important to take things at your own pace, but here are some steps you can take to build your understanding, connection and a sense of empowerment:
- Write down your questions for your next appointment – which treatments are available? What lifestyle adjustments might help?
- Call the Macular Society helpline – get immediate information or clarity on your diagnosis.
- Learn more about your specific type of macular disease – visit our conditions and treatments pages.
- Speak to someone with lived experience – join an online or local support group or request a treatment buddy or befriender through our support services.
- Explore assistive tools – check out our Skills for Seeing resources or low-vision aids to help with everyday tasks.
Other practical tips and advice
Our practical guides cover technology, employment, coping at home, enjoying life out and about, and tips for healthy living, including nutrition.
Frequently asked questions
-
Will I go completely blind?
No. Macular disease affects central vision only. Peripheral vision remains intact.
-
Can macular disease be cured?
There is currently no cure for macular disease, but treatments are available for some types, particularly wet AMD and diabetic macular oedema, that can help slow progression and manage symptoms
-
What treatments are available for macular degeneration?
Treatment varies by type and may include anti-VEGF injections, laser therapy, dietary supplements, or low-vision aids. Your eye specialist will recommend the best option based on your condition.
-
Can I continue working?
Many people with macular disease continue their careers. Get information and advice on reasonable adjustments at work from our Employment pages.
-
Does reading/screen use make it worse?
No. Reading and screen usage don’t harm your eyes. You may find low-vision aids or device settings helpful.
-
Can I drive with macular degeneration?
Yes, if your binocular visual acuity falls below 6/12, you must inform both the Driver and Vehicle Licensing Agency (DVLA) and your insurer.
-
What benefits am I entitled to?
You may be eligible for financial support, including disability benefits and other allowances. Find out what you could claim and how to apply on our Help with benefits page.
-
What nutritional supplements are good for macular degeneration?
Some people with macular disease may benefit from specific vitamin and mineral supplements. Learn more about recommended options on our Nutrition and supplements page.
-
How can I live independently with macular degeneration?
Many people live full, independent lives with macular disease. Assistive technologies and support groups can help you adapt to vision changes and maintain your quality of life.
-
Where can I find support and more information?
You can access practical advice, counselling and local support groups through the Macular Society. Visit our support and treatment pages for more resources and ways to connect.
Join our community at the Macular Society
Become a member today and get your first six months free
From practical tips for dealing with sight loss to the latest research into treatments and a cure; we’re here to help you Beat Macular Disease.
Start your free six months free trial todayLast review date: August 2025